 We’re over one week into our New Year's resolutions, and some of us are already wildly off track. In my household, for example, we are recovering from a whirlwind combination of a sprained ankle, Covid, and pink eye, which means our “to do” lists are completely backed up and any loftier goals feel even further out of reach. Logically, I know health is most important and that the body knows best. So why is delaying my own imagined timeline so inherently frustrating then? It’s multifaceted. American culture promotes an “all or nothing,” fast-paced, quick-fix lifestyle: holiday parties with booze and decadent desserts all December followed by a “dry January” in the gym. Where is the step-by-step middle ground or sick/mental health day factored into all of this? Its absence contributes to a sense of failure when we aren’t able to make progress toward or meet our personal goals right away, especially for those of us with high-achieving, perfectionist tendencies, who love to get things done (which includes myself and most people I support.) The family building journey itself is a seemingly endless moving target of unknown variables starting with the trying-to-conceive process, navigating a complex medical system in hopes of having some semblance of an empowered birthing experience, finding affordable childcare, and then actually parenting and trying to keep the strong-willed little humans you’ve created safe. Keeping ourselves and our offspring healthy during cold and flu season is enough of a challenge, without the added pressure of reaching self actualization through more novel reading, language learning, or muscle building. Yes, striving for personal growth and excellence is important to motivate and anchor our trajectory, but allowing for dips in motivation, unpredictability in scheduling, and other inevitable setbacks should also be factored into our goal-setting timelines. Especially if you’re responsible for someone else’s well-being on top of your own. In art therapy, process is always emphasized over product; the journey vs. the destination. So let’s go easy on ourselves as we ease into 2024. We’ll get there. Post by Sharon Itkoff Nacache ATR-BC LCAT LPAT PMH-C Original photograph by Alessio Soggetti
0 Comments
Throughout human history and culture, symbolic representations of the perinatal experience have been expressed through the Arts, spiritual practices, and ancient mythology. There is a powerful parallel between one’s innate creative process–including conception, incubation/gestation, loss, and rebirth–and a birthing person’s reproductive journey. Unfortunately, today's Western medical model allows little room to explore this connection.
Jung writes, “Initiations bring the realization of a part of the personality which has not yet come into existence but is still in the process of becoming.” Indeed, the birth of a parent is both personal and archetypal, a rite of passage ripe with creative energy and also immense growing pains. Becoming: A Virtual Art Therapy Group for Pregnancy This is a space for gestational birthing persons to explore this intense bio-psycho-social-spiritual transition through a safe, trauma-informed, creative lens. We will be using an open studio process model that is gently structured and allows participants to be both seen and heard through both verbal and creative processing. It requires absolutely no artistic experience other than the availability of basic art supplies and a willingness to try something new. It can be a stand-alone treatment or complement existing individual psychotherapy work. Group goals include: -Creating a sense of community and reducing isolation among birthing people -Allowing a safe space to destigmatize “messy” or ambivalent feelings about becoming a parent -Exploring identity development and new social roles -Developing a mindful practice for distress tolerance and self expression -Cultivating innate creative resilience skills including: role flexibility, creative problem solving, self compassion, and positive reframing Brass Tacks: --Minimum commitment of 4 weekly 1 hr groups to create a sense of continuity for participants -$200/total to be paid by 1/19 via a secure digital platform after a brief phone screening and completion of basic clinical documentation Mon Jan 22 1-2p Mon Jan 29 1-2p Mon Feb 5 1-2p Mon Feb 12 1-2p -Possibility to continue for another cycle depending upon interest -Email [email protected] with questions and to register About Me: I am a mom of two active littles and a perinatal art therapist certified and trained via PSI and Seleni Institute. I’ve been in practice in NYC for almost 15 years and my work has been featured in both the LA & NY Times. I am also a wellness consultant with the Whitney Museum of American Art bringing creative healing spaces to NYC public hospital systems through the HHC Art of Medicine program. To learn more, check out www.cocreatearttherapy.com It’s been a rough year for so many–environmentally, politically, spiritually, personally. Without sugar coating hardship or minimizing the struggle at home or out in the world, I do believe in the power of our experiences to enrich us with the right support. Post-traumatic growth is evidenced by an appreciation of life, ability to relate to others, areas of personal strength, receptivity to new possibilities, and spiritual/existential or philosophical change. I have seen so many examples of this in my clinical work this year and am so grateful to be able to accompany others on their healing paths.
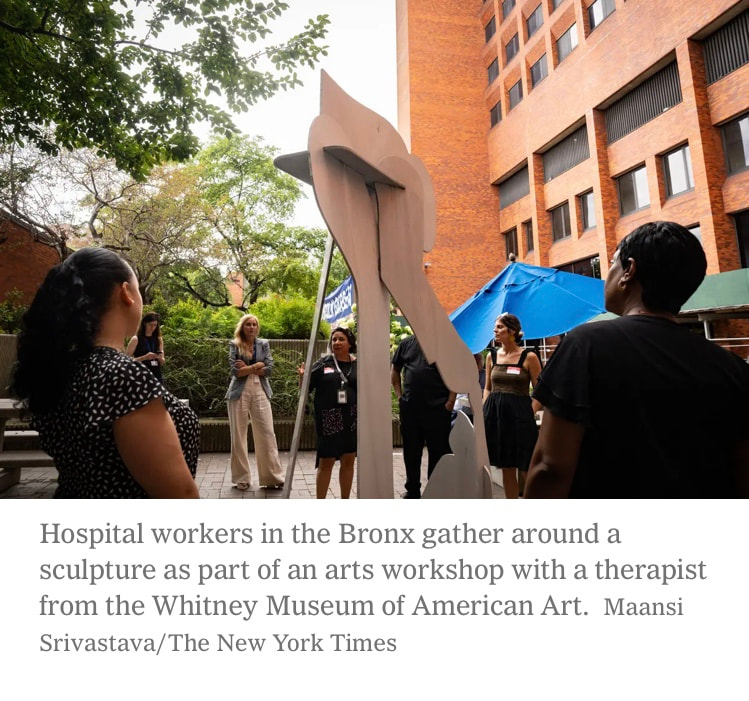
Along with private psychotherapy sessions with expecting/new parents and those contemplating parenthood, this year I’ve been privileged to offer in person, integrative arts-based wellness workshops in 7 NYC public hospitals across the 5 boroughs via the NYC Health and Hospitals HHArt of Medicine program and my ongoing partnership with the Whitney Museum of American Art. With significant experience working with substance use disorders and juggling work with the domestic demands of raising two very active little ones, I am no stranger to burnout syndrome myself. This work fills my cup and fuels me. I feel blessed to be able to provide creative support and psycho-education on both symptoms and prevention, especially for those in caregiving and helping roles. Thank you for entrusting me with your care and please keep me in mind if someone you know is struggling, as I am accepting new clients based in NJ and NY beginning in 2024. Wishing you a safe and healthy new year. #arttherapy #perinatalmentalhealth #caregiverburnout #holidaystress #resilience #posttraumaticgrowth #healing #emotionalsupport #parenting As we stumble onto the rollercoaster that is the December gift-giving season, just a friendly PSA to all my fellow Head of Domestic Affairs, Master Multi-Taskers, and Superhero Parents:
Just because we can do it all, doesn’t mean we have to (or should.) Hallmark-inspired, consumer-driven fantasies around the “perfect” holiday experience, deep-rooted--often patriarchal–-”traditional” gender roles, and perhaps some unconscious desires to either replicate or make up for some lost childhood magic all contribute to the extreme PRESSURE of this time of year. Add flu season, shorter days, year-end work demands, financial stressors, and complex family dynamics to the mix, and we have a perfect cocktail for emotional burnout and all the somatic symptoms (achiness, fatigue, sleep disturbance, frequent illness) that accompany it. So, my advice to not only survive but maybe even enjoy this time of year is simply this: do less and rest more. Delegate wherever possible to lighten the mental load, cut corners, opt out, and give permission to prioritize your own mental, spiritual, physical, and emotional needs first. This may be easier said than done, but it will all somehow, miraculously get done. Maybe not perfectly, but certainly “good enough” and most definitely yours. Besides, our kiddos benefit way more from balanced, present caregivers than frazzled, ragey balls of stress. So, do whatever you need to do to achieve some semblance of that, and do it guilt-free. Your mental health is worth it. Post by Sharon Itkoff Nacache ATR-BC LCAT LPAT PMH-C Original photograph by Annie Spratt  I’ve never considered myself a particularly “political” person, in large part due to privilege but also because I tend to inhabit the healer/peacemaker role, always cherishing individual connections as opposed to larger group opinion. Then I became a mother and I experienced the huge gap in systemic biopsychosocial support once the focus immediately shifts away from the birthing person postpartum, (assuming they had access to quality healthcare to begin with.) Then the pandemic hit, and I experienced the incredible scarcity of economic support for parents, starting with unpaid maternity leave and lack of affordable and sustainable childcare options. I had already been specializing in perinatal mental health and a mom of 2 when Roe vs. Wade was overturned, but it was then that it dawned on me that dedicating my life to supporting women’s wellness is inherently political because women’s bodies have been used as political battlefields throughout history. And we are seeing this play out again and again, especially during last month’s massacre in Israel that included particularly targeted and barbaric acts of violence toward Jewish women and babies. My ears ring with the wail of Palestinian mothers as they, too, weep for the stolen lives of their children. Now it’s not only political, but deeply personal. If politics is defined by power relations and allocation of resources and status, then protecting birthing people’s ability to choose if, when, and how to bear children--and then prioritizing their well-being throughout their lifespans so that they can carry on raising healthy and compassionate individuals--seems to be THE MOST valuable investment of all. So, this is what I remind myself and the young parents I am so honored to work with, when they are inundated with conflicting messages from Tik Tok “university scholars” and overwhelmed with the weight of this burning world that they have worked so hard to bring their babies into. When they are questioning their “first world problems” or what they are doing to make things better or “contribute.” That agonizing over that decision to try again after such a painful loss, that gazing into their infant’s sleepy eyes while chestfeeding through another seemingly endless night, that breaking through patterns of inherited intergenerational trauma in how they parent their own children and learn to re-parent themselves, is not only “doing enough,” but, in fact, revolutionary. And that this job is, in fact, the most important, challenging, and humbling one, even if modern civilization has yet to protect the sanctity of this. #realtalk #perinatalmentalhealth #reproductiverights #motherscall #collectivegrief #politics Post and Image by Sharon Itkoff Nacache ATR-BC LCAT LPAT PMH-C
So, how do we approach this holiday that celebrates all that is primal, scary and grotesque when real life already contains enough horror, anxiety, and reminders of suffering as it is?
Personally, I am experiencing a kind of dissonance around the macabre/horror themes. Right now skeletons and bloody characters presented as lighthearted fun feels too triggering, too real. But I’m also aware of the importance of being able to “play” with the death anxiety we all share, especially in safe contexts. Although this is a universal, often unspoken fear that connects us all, naming it is completely taboo in our death-denying, youth-obsessed, toxic positivity culture. So instead, we avoid it altogether, relegate it to one holiday a year, or save it for funerals, news, and obituaries. Author Ruth Soukup remarks, “Fear is a funny thing... The very instinct designed to protect us also holds us back.” Indeed, in small doses, leaning into our fears and being “counterphobic” can offer practice in diffusing and eventually overcoming them. This includes digging into aspects of ourselves that are less desirable or “unknown.” Drama therapy theory emphasizes the importance of role flexibility on mental health: the ability to wear many hats, evolve, and exercise many aspects of ourselves as opposed to staying stuck in one, fixed role. In a safe context like ongoing therapy or through one’s artistic practice, becoming acquainted with the “shadow side” or darkness within ourselves can be a vital part of both self discovery and healing. #halloween #currentevents #arttherapy #shadowside #deathanxiety Post by Sharon Itkoff Nacache ATR-BC LCAT LPAT PMH-C Pumpkin design by author’s son Today, on World Mental Health Day, with so much of the world grappling from personal and global challenges that directly impact their loved ones or their own sense of wellbeing and safety, I am reminded of the power of art to express what it means to be human. And connecting to that humanity, within ourselves and one another, is inherently healing.
Susan Magsamen, the director of the International Arts+Mind Lab at Johns Hopkins University School of Medicine, reflects on the vulnerable and humbling experience of hospitalization, and how this can be “one of the most stressful experiences anybody ever has.” The Arts in Medicine department of New York City Health and Hospitals was developed in 2018 as part of a growing movement in healthcare to utilize the arts for healing. Their collection of artwork set in public spaces around hospital facilities across the boroughs helps “create an enriched environment that can lower stress, anxiety and blood pressure, improve moods and lead to faster healing.” I feel honored to be able to collaborate with NYC Health + Hospitals and the Whitney Museum of American Art and implement a deeply personal, art-centered approach to care through ongoing arts-based wellness workshops. This approach focuses on close-looking dialogue and creative resilience skill-building to help hospital employees in every role cultivate self compassion, build community and camaraderie, alleviate symptoms of burnout, and develop mindful stress management tools on the job. Photos of the program and more about the history, impact, and vision of the program are featured here: https://www.nytimes.com/2023/10/08/nyregion/nyc-hospitals-public-art.html Post by Sharon Itkoff Nacache ATR-BC LCAT LPAT PMH-C Creative Support for Caregivers is a virtual art therapy group using an open studio process for anyone in NJ/NY who identifies as a caregiver and is interested in developing a restorative creative practice for stress management. Whether it is someone in a helping profession, the “giver” or “caretaker” in a romantic relationship or among one’s social group, a parent of younger child(ren), older child of an elderly parent, or those “sandwiched” in between, this is THEIR creative space. Group objectives include:
 |






 RSS Feed
RSS Feed